Dr. Chandana Choudhury Baruah
Professor, Department of Pharmacology & Toxicology
College of Veterinary Science, AAU, Khanapara, Guwahati-781 022
If you are in the teaching line, you should always be in touch with the current topics or treatments if you are a physician. Hence, a new term recently I have come across in Readers’ digest intrigued me. It is much deeper than I thought. However, targeting a drug with bacteria or virus is somewhat fascinating. Most of us suffer from stomach upset, and doctors name them as Irritable bowel syndrome, Crohn’s disease, GERD, even colon cancer, if it is not detected or diagnosed properly. This creates havoc in one’s life, as no drug, lifestyle change, yoga, or allopathic medicine can help them.
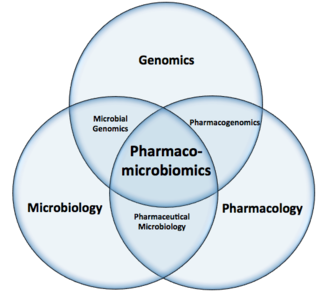
The problem so far is taken care by the conventional treatment. But with the new concept of omics, here come few saviours. Scientists or researchers are still trying to understand and personalise the treatment. Pharmacomicrobiomics is such a new horizon where atleast some hopes are palpable.
Individual responses to a specific drug vary greatly in terms of both efficacy and toxicity. Inter-individual variability in the drug response thus affects not only the patients’ well-being, it also poses an enormous clinical and financial burdens. For the development of “personalized medicine”, it is therefore crucial to determine how we can assess a patient’s probable response to a drug, increase drug efficacy and reduce the risk of ADRs.
Pharmacogenetics and pharmacogenomics have been at the forefront of research examining the impact of individual genetic make-up on drug response variability. It has now been estimated that genetic factors could explain 20% – 95% of the variability in response to an individual drug. But that is not all.
Now, the gut microbiota has emerged as an “organ” that plays an important role in health and disease. The human gut harbours thousands of different bacterial species and other microorganisms that form a complex ecosystem. The composition of the gut microbiome shows a high inter-individual variation that is associated to a number of host and extrinsic factors. Various studies in mice and humans have shown the effect of drug intake on the gut microbiome. In turn, the gut microbiome can also contribute to an individual’s response to a specific drug: the microbial community in the gut can modify the pharmacodynamics of a medication by directly transforming the drug or by altering the host’s metabolism or immune system. Don’t we suffer from stomach disorders after taking antibiotics? Doctors now- a-days either prescribe probiotics or some medicines already available with probiotic, just to protect the useful bacteria in our gut.
The term pharmacomicrobiomics describes the influence of microbiome compositional and functional variations on drug action, fate and toxicity. The gut microbiome is emerging as an essential component in the development of personalized medicine and modulating the gut microbiome has the potential to become a very attractive approach to managing drug efficiency and safety on the level of the individual.
A medicine may pass through the upper GI tract and small intestine into the large intestine, where they come in contact with the thousands of microbial species that reside in the human gut. Complex drug-microbial interactions occur mainly in the colon. Drugs may change intestinal microenvironment, alter microbial metabolism or affect bacterial growth, thereby altering microbial community composition and function. On the contrary, the gut microbiome can also participate directly in chemical transformation of drugs. In the host, drug metabolism occurs predominantly in the liver and can be divided into two phases of reactions: modification and conjugation. Upon metabolism in the gut and/or the liver, drug metabolites are either transported to targeted tissues or excreted by the kidneys into the urine or by the liver via the biliary system back into the gut lumen. In the gut, drugs or their drug metabolites can be subjected again to bacterial metabolism. This complexity means that pharmacological studies require a systems biology approach that considers drug-related hepatic and bacterial metabolic processes, as well as complex host-microbe-drug interactions.
Effects of antibiotics on the gut microbiome are the most studied, and antibiotic-induced dysbiosis (opposite of symbiosis) in the gut microbiome can increase susceptibility to infections, compromise immune homeostasis, deregulate metabolism and obesity. While majority of the current findings are association-based, the identification of a causal impact of proton pump inhibitors (PPIs), which are used to treat gastro-oesophageal reflux and heartburn, and the anti-diabetic drug metformin on gut microbiome composition provide firm evidence that alteration in the gut microbiome should be considered when evaluating drug safety and that drug use can also confound microbiome analysis.
Metformin is an antidiabetic for type II diabetes, and the beneficial impact of metformin in regulating the structure and function of the microbiota is emerging. According to Forslundet al. (2015), metformin could increase the abundance of bacteria that produce short chain fatty acids (SCFA), and these could mediate the therapeutic effects of metformin.
One representative example of the microbial impact on drug bioavailability is seen for simvastatin, a drug commonly prescribed in the treatment of hyperlipidaemia. Plasma concentrations of simvastatin are positively associated with microbially synthesized secondary bile acids (Kaddurah-Daouket al.,2011). Since bile acids are important agents for intestinal nutrient absorption, this also may determine the absorption of simvastatin into the host and influence the drug’s bioavailability.
The gut microbiome is thus emerging as an important player in personalized medicine. Notably, in contrast to human genetic make-up, the gut microbiota can be modulated. Pharmacomicrobiomics thus may have at least two global clinical applications: 1) to combine personal microbiome and genetic profiles to better predict an individual’s medication response, and 2) to modulate the gut microbiome to improve drug efficacy on the individual level. To achieve this, a systems-based approach and individualized drug testing systems are needed to further understand the underlying causalities and mechanisms.
References:
Forslund, K; Hildebrand, F.; Nielsen, T. et al. (2015).Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature. 528(7581): 262-266.doi: 10.1038/nature15766.
Kaddurah–Daouk,R.; Baillie, R.A.; Zhu, H.; Zeng, Z-B; Wiest, M.M.; Nguyen, U.T.et al. (2011). Enteric microbiome metabolites correlate with response to simvastatin treatment. PLoS One, 6(10): e25482.