Kanjanabh Kumar Das
3rd Year B.V.Sc. & A.H.
College of Veterinary Science, AAU, Khanapara, Guwahati-22
Man and animal have shared this earth together since time immemorial. As such, they have been part of a system larger than life, comprising all life. This thriving, flourishing system made up of biotic and abiotic components is what we call an ‘ecosystem’. Humans, animals and their environment are all a part of that ecosystem, and thus are intertwined & interdependent. The realization of this interdependency and “one cause-multiple effect” concept has led to the genesis of ‘One Health’ practices.
What initially started as a “survival of the fittest” eventually turned into a deep symbiosis among the factions. Since the Old Stone age, man hunted (animals) and foraged (plants) for food. With time, each faction evolved their own defense mechanisms in order to protect themselves. This led to several conflicts, with one falling victim to the other. As civilization dawned over ‘the Fertile Crescent’ in around 8000 BC, the process of domestication started, followed by agricultural practices. The dog was the first animal to be domesticated (for protection), followed by the goat (for production). The domesticated animals depended on man for their care and man depended on these animals for their services. Eventually, man started breeding them and produced successive generations with suitable characteristics to best fit their aim. In a similar fashion, the early man discovered that agriculture is a much more efficient means of securing food for themselves and feed for their livestock. Thus, the early nomadic man finally settled down, leading to several changes in society, economics, food habits, and the topic of discussion- disease and treatment.
Mankind has fought several wars throughout the ages. The ideology of “If you want peace, prepare for war.”- is at the core of the human race, as witnessed throughout the pages of history. But for a considerable amount of time, there was one enemy that mankind had no triumph over – one which killed millions in ways unheard of. This was initially speculated to be the doing of demonic or supernatural entities, as evident by the demonic theory of disease. But as biomedical science developed, that enemy was found to be none other than the infectious bacteria, viruses, parasites, fungi and other agents which stroke swiftly and killed cruelly. The early man had many indigenous ways of dealing with these diseases, probably through the use of some naturally occurring antimicrobials, as they have been present in nature long before we learnt of them. Thus, the concept of healthcare before antimicrobials solely relied on the individual’s immunity and supportive therapy. But with the discovery of the first antimicrobial Penicillin way back in the year 1928, we harnessed the power to strike back at our microscopic invaders. Thus began an era of antimicrobials and chemotherapy, spearheading the elaborate war on the microscopic front.
Antimicrobials (anti: against; micro: microorganisms) is a broad term that encompasses all substances used to treat microbial infections, including antibiotics, antifungals, antivirals & antiparasitics (Martino, 2022). They are pharmacologically active substances which act by killing (e.g.: bacteriocides) or retarding the growth (e.g.: bacteriostats) of microorganisms. They target key steps of cellular metabolism and act by deactivating molecular synthesis, inhibiting enzyme function or destroying important structures such as cell walls or biomembranes. Antimicrobials are always used in a living system, as opposed to disinfectants, which are applied on non-living surfaces. Antimicrobials have been extensively used for their therapeutic properties, for treatment of various diseases and ailments. When paired with efficient vaccination and management practices, antimicrobials have even led to complete eradication of some diseases. They hold extreme importance in the veterinary sector also, not only for their therapeutic applications but also for their effects on production.
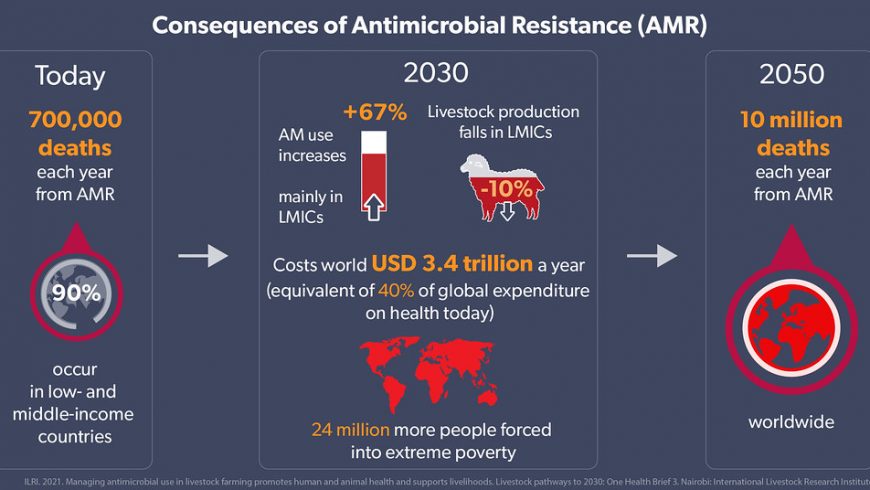
Unlike agriculture, which is comparatively easier to practice organically, animal husbandry is seldom practicable without the use of prophylactic measures including preventive medication and vaccination. This is due to the fact that in a country like ours, where most of the farmers are marginal, strict biosecurity measures are often sacrificed due to a financial lacuna, making the animals more susceptible to disease outbreaks. In the light of such an outbreak, antimicrobials are employed by the farmers or veterinarians in order to save his/her animals. Sometimes, such farmers, fearing a loss of productivity and consequent finacial loss during outbreaks, employ antimicrobials haphazardly before the disease has even occurred. This injudicious method of prophylaxis is often effective at the first glance but comes with tremendous costs. The end result is that a disease hits harder, stays longer and is extremely difficult to cure, bringing along heavy economic losses in the long run. This is the gist of the current burning problem of Antimicrobial Resistance or AMR.
“What doesn’t kill you makes you stronger”- such is the idea behind antimicrobial resistance. Resistance can be caused by a number of practical scenarios, but the end result is always the same- the microbial agent becomes stronger than the antimicrobial drug, so much so as to nullify its effects and thrive in its vicinity. There is a change in the genetic level of the pathogen, which can occur slowly or abruptly. When the drug is potent enough to affect the genetic structure of the organism (mutagenicity), but the dose is low enough not to perform its desired therapeutic effect, i.e., to kill the agent in question, resistance prevails. Fast changes, called mutations, can induce resistance quickly, so much so as in the same generation of pathogens that lived when the drug was administered. However, evolutionary changes are slower, conferring resistance upon the microorganisms after one or two generations have passed. On a broad scale, this is usually not a problem as the generation time between two successive generations can be quite small for these microscopic creatures (e.g.: E. coli with a generation gap of only about 20 minutes).
Regarding the ways that could lead to antimicrobial resistance, one could debate – it is more or less due to the lack of awareness, and can be boiled down to the following points:
- Wrong dose of the right drug: An antimicrobial is prescribed after a proper assessment of the microbial load, disease progression and the health status of an animal. Therefore, when we administer a lower than required dose, the drug loses its desired effect of eradicating the infection. Moreover, it sensitizes the pathogenic agent to the drug. The same drug, when repeated later, requires an even higher dose to be administered or might be futile altogether.
- Administration of the wrong drug: A drug should be administered after a proper investigatory study of the pathogens present in the clinical samples. Administration of random drugs has dual effects: the first being a non-existent therapeutic effect, which might even range to an adverse effect, and the second – sensitization of the existing microbes, resulting in resistant ‘superbugs’.
- Leaving the antimicrobial treatment course unfinished: An antimicrobial agent is required to be present in circulation in a specific concentration for a specific period of time for the desired results. Most farmers stop using the drugs when the signs and symptoms disappear, with the illusion that the animal has recovered. But it prepares the existing microbial load to produce a more severe infection the next time the conditions get favourable for them.
- Haphazard use of drugs as a preventive measure: A rule of thumb is that antibiotics should not be used as prophylactics. Even if they are used, there is a definite time frame in which all production (e.g.: milk) from the animal should be discarded. But in conditions like ours, due to either ignorance or unaffordability, such practices are not followed, leading to antimicrobial residues seeping into milk and meat, which are then consumed by humans. This is one of the major ways through which AMR spreads.
- Using antimicrobials when other measures are just as effective: Often the use of antimicrobials can be substituted for a simple application of biosecurity or control measures. If a farmer detects that an animal is sick, it should be isolated from the rest of the herd in order to stop the spread. Advocating quarantine for a new stock, at least for the minimum recommended duration for the species, is a necessity. In a similar fashion, adoption of strict biosecurity protocols like restriction on entry/exit, record keeping, foot baths, hygiene & sanitation, etc. are the need of the hour.
- Unethical Practices: Giants of the pharmaceutical industry often endorse their products (antimicrobials) by providing several benefits to doctors who prescribe their drugs. Such companies often set a quota for their doctors, which results in unethical prescription of the said antimicrobials in return for a favour or reward. This is a severe problem in its own right and should be tackled effectively.
- Drug Abuse: Another reason for antimicrobial resistance, which deals more with the human aspect of One-Health, is drug abuse. Non-sterile, injudicious and unlawful intake of drugs for personal pleasure leads to resistance to the particular drug, among a plethora of other health issues. Availability of antimicrobials across the counter without a prescription itself is unethical and therefore banned in many developed countries.
Keeping the above facts in view, one can understand that antimicrobial resistance is a global, all-encompassing problem. It strengthens the environmental pathogens, which affect the animals, leading to problems in humans. Thus, in the present day context, AMR is a grave challenge to the One-Health alliance, and veterinarians are needed to play a pivotal role in combating it by adopting the following measures.
- Inspection: Stringent inspections of the global livestock products trade, antibiotic residue testing, and sustainable organic farming education are important duties that the veterinarians must carry out diligently.
- Standards: Setting up, following and updating species-specific standards and rules regarding antimicrobial administration, whenever necessary, holds utmost importance in clinical practice.
- Cooperation: Efficient alliance among doctors, veterinarians, scientists, environmentalists and animal welfare experts would help spread the facts and concerns about the ill-effects of antimicrobial resistance, which in turn would help educate the people.
- Legislation: AMR is a global problem, comparable to the climate change. Governments all throughout the world would soon be required to form new laws or update existing ones against unethical prescriptions, malpractice, illegal livestock trades, corruption at various levels of livestock production, and so on. Moreover, the administrative machinery should be able to impose these laws with an iron hand.
- Economy: In order to follow these rules and still make a generous profit, farmers should be educated and uplifted, right from the grassroot level. Various incentives may be provided by the government to the cooperative farmers, and the government should work closely with veterinarians in order to discover new effective ways of sustainable livestock rearing in the country minimizing the possibility of occurrence and spread of infectious disaeses.
All in all, education and implementation should be at the core while solving the burning problem of AMR. Although much can be discovered in the near future, the time to act is now. It is a slippery slope, and even time is slipping out of our hands. It is rightly said that “With great power comes great responsibility.”- because while it is true that antibiotic resistance is a complex issue, the reasons as to why antimicrobial agents are a vital part of healthcare are simple, straightforward, and backed by the belief that they must always be used responsibly.
References:
Martino, P.D. (2022). Antimicrobial Agents and Microbial Ecology. AIMS Microbiology, 8(1): 1–4, DOI:10.3934/microbiol.2022001.
Quinn, P.J.; Markey, B.K.; Leonard, F.C.; FitzPatrick, E.S.; Fanning, S. and Hartigan, P.J. (2011). Veterinary Microbiology and Microbial Diseases, 2nd edition. Wiley-Blackwell, New Jersey.
World Health Organization (2023). Antimicrobial Resistance, Retrieved on 8th Nov. 2023,
(https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance).