HiuenTsang Mochahary, Ankita Choudhury, Arpita Bharali, Nagendra Nath Barman and Lukumoni Buragohain
College of Veterinary Science, Assam Agricultural University, Khanapara, Guwahati, Assam
Introduction
The year was 2019; little did we know that the world was totally unprepared for what was to come. The world came to a sudden halt. The 21st Century was facing its biggest medical challenge at a global level due to the COVID-19 pandemic. As the world is still under the pressure of COVID-19 outbreaks, another outbreak has emerged in the form of monkeypox. The simultaneous outbreak drew the attention of the public health officials as to whether it would pose a new threat to the mankind.
Monkeypox (Mpox) is an infectious viral zoonotic disease which is encountered in humans and other animals such as squirrels, dormice, rats, some non-human primates and many other species. Symptoms usually start at around 3 weeks after coming in contact with the virus and development of rash starts 1-4 days later. People infected by this disease exhibit symptoms similar to smallpox such as fever, shivering, rash and swollen lymph nodes which eventually turn into blisters and crusts over. Rash, which look like pimples or blisters and can be itchy, and is usually seen on the hands, feet, face, around genitals and anus. They last for around 2-4 days before drying up, crusting and falling off. However, unlike the smallpox infection, rash is milder and the disease causes lower mortality rate. Complications due to Mpox infection may include blindness, severe scars on the face, arms, and legs and in rare cases, and death. Most of the patients recover within a few weeks even without treatment.
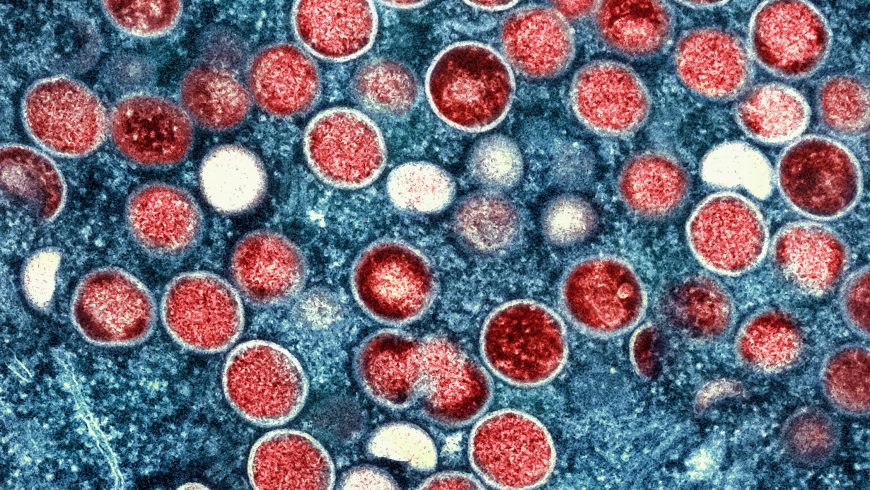
Monkeypox virus, of the Poxviridae family and the genus Orthopoxvirus, is the causative organism of monkeypox and is a double-stranded DNA virus. This Orthopoxvirus is closely related to other pox viruses namely variola, vaccinia and cowpox viruses. The genome of monkeypox virus is around 197 kb long and is comparatively larger than other viruses.
Monkeypox has earned its name as the virus was first isolated and identified in 1958 from laboratory monkeys during an outbreak in an animal facility in Copenhagen, Denmark, although most of the carriers of this virus are rodents. The natural history of the virus remains uncertain and further studies are needed to ascertain its exact reservoir. The Democratic Republic of Congo reported the first case of confirmed human Mpox infection in 1970 (Ladnyj et al., 1972).
Eradication of smallpox and lack of vaccination efforts is one of the factors to have contributed to the rise of Mpox outbreaks. Monkeypox is primarily known to occur in the rural regions of Central and West Africa with the infection now rapidly spreading to the urban areas. It has been divided into two clades: one from the Congo Basin (Clade I) and the other from the West Africa region (Clade II). The former clade is known to be more virulent. The recent outbreak has been classified under Clade II.
Host and Transmission pattern
Monkeypox is zoonotic in nature, i.e., it can be transmitted from animals to human by direct contact with the infected animals’ blood, mucosal or cutaneous lesions, and body fluids. In humans, it can be transmitted by sharing common objects like towel, clothing, etc. Though the natural reservoir of this virus has not been identified yet, evidence of the presence of this virus in various animals has been observed in Africa. Examples are rats, monkeys, squirrels, and non-human primates. The first case of Mpox was reported in macaque monkey but rodents and other small mammals have been spreading the virus widely. Apart from being transmitted from animals to humans, human-to-human transmission occurs through droplet respiratory particles when they are in close contact. The monkeypox virus can also be transmitted from the mother to the foetus via the placenta.
Clinical signs and symptoms:
This is a self-limited disease; symptoms can last for 2-4 weeks. The incubation period of Mpox virus ranges from 5 to 21 days. The early symptoms are raised spots that later turn into fluid-filled blisters. The infection occurs in two stages: the first one lasts for 0-5 days, also known as the invasion period. The initial symptoms can be similar to that of chicken pox or measles which include fever, back pain, headache, swelling of the lymph nodes, myalgia and lethargy. The second stage generally starts 3 days post onset of fever. Skin eruptions and rashes begin to appear all over the face. Rashes can also occur on the palm, feet, genitalia, conjunctivae, and cornea in some cases. The rash starts from being flat to being filled with pus. Fatal cases have been seen more frequently among children with a recent ratio of 3-6%. Besides the aforementioned symptoms, the Centre for Disease Control and Prevention (CDC) has also suggested looking for infected Mpox individuals with sexually transmitted infections as co-infections with herpes, syphilis, chlamydia and gonorrhoea have been reported.
Status of the recent outbreaks
After the global eradication of smallpox in the 1970s, the monkeypox virus took the spotlight. It was not until the 2003 US outbreaks that Mpox truly gained the global attention. The biggest outbreak till date occurred in Nigeria in 2017. Most of the cases confirmed to contract monkeypox infection had a recent travel history to European and North American countries instead of West or Central Africa, where Mpox is known to be endemic. The CDC has confirmed 5783 monkeypox cases as of July 1, 2022 spread over 52 countries. Most infected individuals are male and in their 40s, the reason behind this is yet to be known. Mpox infections were also found in individuals with no direct travel links to the infected countries. Gradually, cases began to surface from all across the globe and as a result, the World Health Organization (WHO) declared monkeypox as a global public health emergency. The CDC data reveals that by January 2023, 110 member states across six WHO regions reported a total of 85,922 confirmed Mpox cases including 96 deaths.
Prevention and Treatment
Monkeypox transmission can be mitigated through implementation of proper prevention and control measures. There is no known cure for monkeypox and hence most treatment is aimed at relieving symptoms. Owing to cross-protection offered by the vaccines based on vaccinia virus and smallpox, monkeypox vaccines have been developed based on those formulations. A study conducted in 1988 showed that the smallpox vaccine was 85% effective in protecting and lessening the severity of the disease (Fine et al., 1988). More recently, another vaccine has been developed based on the Ankara strain. It is a two-dose vaccine which had been approved in 2019. Furthermore, if smallpox vaccine is administered 3-5 years before coming in contact with the disease, monkeypox infection can be prevented. Other medications may include use of antiviral drugs like Brincidofovir or Tecovirimat and vaccinia immune globulin.
Some of the preventive steps that can be exercised to prevent Mpox are:
- Avoiding skin-to-skin contact with people having rash that looks like that of Mpox.
- Avoiding handling of clothes, sheets or materials that have been used or in contact with an infected person or animal.
- Keeping Mpox diagnosed people isolated from the healthy ones.
- Frequently washing hands with soap or usingalcohol-based sanitizers.
- Getting vaccinated.
- Avoiding animals that are potential carriers of the virus.
Additionally, since health workers are at a high risk of contracting the virus, extra precautions like using a PPE kit and proper handling of the suspected Mpox infected sample should be exercised. Gloves should be used for direct contact with the lesions of Mpox. Unprotected contact with wild animals must be avoided. Furthermore, since most of the confirmed cases have occurred in young and middle-aged men who have had recent sexual encounters, WHO recommends reducing the number of sexual partners and reconsidering sex with new partners.
Conclusion
The sudden outbreak of monkeypox virus in endemic and non-endemic places has raised global concern. Although monkeypox was previously endemic to the regions of Africa, it has managed to become a disease of global concern. Studies are ongoing as to understand and identify its natural reservoirs and the cause of occurrence of outbreaks in depth. The WHO and the CDC have suggested certain measures to prevent contracting the disease . The increase in the number of cases has made it imperative to determine the route of infection and creating awareness to prevent the disease. Furthermore, the simultaneous outbreak of COVID-19 and monkeypox has exposed the shortcomings of the healthcare system across the globe, and the lack of awareness among the people. There is an immediate need to upgrade our healthcare systems creating awareness among the masses and the need for hygiene to tackle such health risks to combat other probable emerging or re-emerging deadly viruses in future.
References
- CDC (2023). cdc.gov/poxvirus/monkeypox/prevention/protect-yourself.html (Retrieved on 07.03.2023).
- WHO (2023). https://www.who.int/news-room/fact-sheets/detail/monkeypox (Retrieved on 07.03.2023).
- Fine, P.E.; Jezek, Z.; Grab, B. and Dixon, H. (1988). The transmission potential of monkeypox virus in human populations. International Journal of Epidemiology. 17 (3):643–650.
- Ladnyj, I.D.; Ziegler, P. and Kima, E. (1972). A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bulletin of the World Health Organization. 46(5), 593–597.