Christine Vanlalbiakdiki Sailo and Nachimuthu Senthil Kumar
Department of Biotechnology
Mizoram University (A Central University)
Aizawl – 796 004, Mizoram
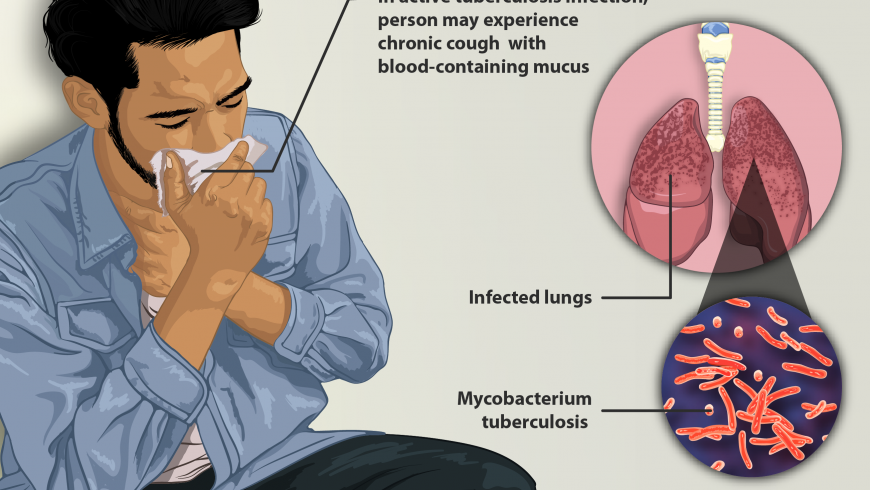
Mycobacterium tuberculosis, a contagious disease, has been hypothesized to live and evolve with mankind for more than 150 million years. More than a century has passed from the day of its discovery by Robert Koch and till date mankind is unable to eradicate this deadly disease plaguing human. The National Strategic Plan (NSP) set out the strategic direction and key initiatives to be undertaken under the Ministry of Health and Family Welfare, Govt. of India from 2017 to 2025 for working towards achieving the goals of eliminating TB by 2025.
In the modern world, we now know that tuberculosis is a multifactorial disease, and many factors contribute to the outcome of the disease. Global TB report 2022 estimated that 10.6 million people fell ill with TB in 2021, an increase of 4.5% from 10.1 million in 2020. In India, the total number of incident TB patients (new and relapse) notified during 2021 were 1.93 million as opposed to that of 1.62 million in 2020.
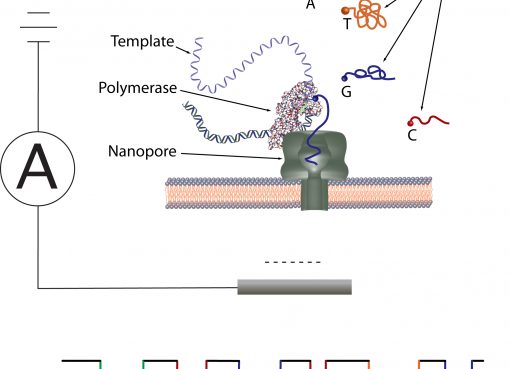
Mizoram is a small, hilly tribal state, situated in the northeastern region of India, sharing international borders with Myanmar and Bangladesh. It is the least populous state in India after Sikkim. The projected population for Mizoram in 2023 is 13.80 lakhs. As per India TB report, in 2021, as many as 1,749 TB cases had been notified from both public and private sector (82.7% new cases, 10.9% previously treated, 6.4% drug resistant TB). In 2003, Mizoram implemented RNTCP (Revised National Tuberculosis Control Program) and PMDT (Programmatic Management of Drug Resistant Tuberculosis) which is the former DOTS Plus in 2011. Currently, among the laboratory tests available for TB, smear microscopy along with Xpert MTB/RIF assays are the only diagnostic tools implemented in the state. Xpert MTB/RIF is being utilized by Mizoram since the end of 2014 and it is among the few states in the country where Universal Drug Susceptibility testing using Cartridge Based Nucleic Amplification Test (GeneXpert) was implemented from 2017. This is a nationwide programme to test every TB patient for signs of resistance to the first-line drugs, especially Rifampicin.
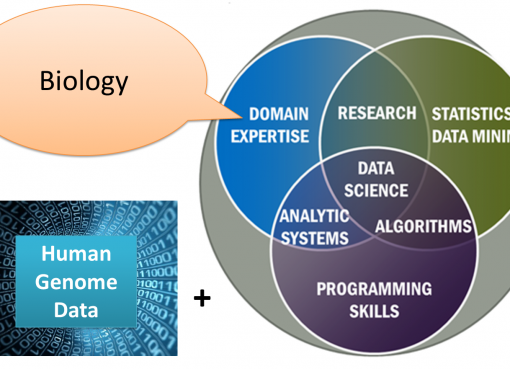
A few studies on TB were conducted under a project sponsored by DBT, New Delhi to help establish a baseline data as well as to explore the status of TB in Mizoram in terms of host and pathogen genomics along with epidemiological factors involved. Arguably, there are no scientific reports or evidence on host mitochondrial genetic factors linked to TB, though mitochondrial DNA (mtDNA) variations have been established for different diseases including different types of cancers. The entire mitochondrial genome from blood samples of Mizo TB patients and healthy controls were analyzed to understand the possible mtDNA variants. The potential impact of non-synonymous substitutions on protein functions were determined using prediction tools (Polyphen-2 and Provean). A total of 28 non-synonymous variants were found, of which 2 variants (MT-ND2 g. A>G4824 p.T119A and MT-ND6 g. T>C14180 p.Y165C) were found to be deleterious among the cases, significance of which is yet to be understood. Majority of the variants lies in the D-loop of the non-protein coding region of the mtDNA. We propose that mutations in the mitochondrial genome need to be validated further using functional studies to understand their association with TB.
Similarly, pertaining to epidemiological or demographic risk factors involved in TB, little information is available from the North-Eastern Region of India. Though various risk factors of TB have been studied across the globe, in view of the fact that they may be altered over time and may have geographic specificity, data collection from TB patients as well as healthy controls based on a structured questionnaire was done to analyze the presence of any less-established risk factors. Clinical presentations like fever, cough, weight loss, chest pain and night sweats were more common among the pulmonary TB patients. The most common mode of diagnosis among pulmonary and extrapulmonary TB were Xpert MTB/RIF and X-ray, respectively. TB was found to be significantly prevalent among people from lower socio-economic status, less educated, unemployed, and improper housing conditions. Other risk factors associated were alcohol consumption, neighbours with TB, travel history, no BCG vaccine uptake, mass gathering and non-ideal weight (under and overweight). An interesting less-established risk factor that demands attention is the domestic source of water supply (river & spring water) which was found to be significantly associated with TB in our study. Though TB is well known for its air borne transmission, other possible routes of transmission are in question or rather debatable. Water supply for domestic purpose is yet another important aspect that is often neglected in the recent studies pertaining to TB transmission. It is speculated that apart from all the well-established risk factors for TB, water supply might play a crucial role towards transmission of TB, since hospital liquid waste treatment is yet to be adopted in Mizoram. Our previous 16s rRNA metagenome study had also reported the pollution of soil and river ecosystems in Mizoram by the discharge of solid and liquid wastes from domestic, municipal, and hospital premises, where apart from other pathogenic bacterial communities, Mycobacterium tuberculosis was also found. From a public health standpoint, this is alarming and highlights the need for further research in this area.
As mentioned earlier, Xpert MTB/RIF being the mainstay of laboratory diagnosis within the Mizoram state, a retrospective study was conducted for Rifampicin Resistant TB (RR-TB) cases from archived results for all the specimens received during 2014 to 2021. Among these, the proportion of RR-TB diagnosed was 15.9%. The most affected age group observed was productive individuals between 25 and 34 years. Among the RR-TB cases, 57.8% were males and 42.2% were females. Higher DNA amount was observed in pulmonary cases (sputum) while low/very low amount of DNA was common among extrapulmonary cases. Rifampicin being a surrogate marker of multi-drug resistant TB, the rpoB gene of Rifampicin utilized by the Xpert system spans across five overlapping probes namely: Probe A (codons 507-511), Probe B (codons 511-518), Probe C (codons 518-523), Probe D (codons 523-529) and Probe E (codons 529-533). The rpoB gene mutations recorded in Mizoram were as follows: Probes A (25.9%) followed by E (23.5%), D (9.8%), B (2.6%) and C (0.2%). In addition, high prevalence (34.3%) of probe mutation combinations were also found: probes AB (0.4%), AD (32.8%), AE (0.4%), DE (0.2%) and ADE (0.4%). The frequency of probe mutation combinations also increased from 2014 to 2021. Through this study, it was also observed that the order of the probe mutation found in Mizoram varies from that of other similar studies conducted within and outside India.
Liquid culture using Mycobacteria Growth Indicator Tubes (MGIT) was also carried out which showed phenotypic drug susceptibility as: Streptomycin (57.1%), Isoniazid (51.8%), Rifampicin (64.3%), Ethambutol (57.1%), and Pyrazinamide (39.3%). Further molecular work was performed including Long Sequence Polymorphism (LSP-PCR) which showed the presence of four lineages in Mizoram: Lineage 1(Indo-Oceanic), Lineage 2 (Beijing), Lineage 3(East-African Indian) and Lineage 4 (Euro-American). Mixed lineage infection of Lineage 1 and Lineage 3 were also seen in two patients. Sanger Sequencing revealed the mutation in Probe A region as L511P (CTG>CCG) and Probe D region as H526Q (CAC>CAG) and H526L (CAC>CTC). The L511P and H526Q mutations were seen in new and treated cases. Discrepancy was also observed between MGIT drug susceptibility and Xpert MTB/RIF.
Our study provides genetic pattern of drug resistance accountable for Rifampicin Resistance over the past years in Mizoram which might help local clinicians in the initiation of correct treatment. It also provides a baseline data on the magnitude of RR-TB within the state. Utilization of sequencing technologies is essential in diagnostic laboratories to rule out discrepant results and as a cautionary measure to prevent wrong diagnosis and treatment. Identification of the residential areas can help local health authorities and policy makers in planning effective surveillance programs to control the spread of RR-TB within the state.
Acknowledgement:
The authors thank all the collaborators and the Department of Biotechnology (DBT), New Delhi for financial support for this work under the MDR -TB NER Project (BT/PR23092/NER/95/589/2017).
References:
Vanlalhruaii Tonsing, M.V.; Sailo, C.V.; Sanga, Z.; Chhakchhuak, L.; Chhakchhuak, Z.; Pandit, B.; Kumar, D.; Mazumder, P.P. and Senthil Kumar, N. (2020). Analysis of variants in mitochondrial genome and their putative pathogenicity in tuberculosis patients from Mizoram, North east India. Mitochondrion 54: 21-25.
Sailo, C.V.; Tonsing, M.V., Sanga, Z.; Chhakchhuak, Z.; Kharkongor, F.; Fela, V.; Chhakchhuak, L.; Ralte, L.; Nemi, L. and Senthil Kumar, N. (2022). Risk factors of tuberculosis in Mizoram: First report of the possible role of water source. Indian J. Tuberculosis 69(4): 675-681.
Sailo, C.V.; Zami, Z.; Lalremruata, R.; Sanga, Z.; Fela, V.; Kharkongor, F.; Chhakchhuak, L.; Chhakchhuak, Z.; Laldinmawii, G.; Kumar, D. and Senthil Kumar, N. (2022). MGIT sensitivity testing and genotyping of drug resistant Mycobacterium tuberculosis isolates from Mizoram, Northeast India. Indian Journal of Medical Microbiology 40(3): 347-353.
Sailo, C.V.; Ralte L.; Sanga, Z.; Fela, V.; Kharkongor, F.; Chhakchhuak, Z.; Chhakchhuak, L.; Nemi, L.; Zothanzama, J. and Senthil Kumar, N. (2022). Distribution and frequency of common mutations in rpoB gene of Mycobacterium tuberculosis detected by Xpert MTB/RIF and identification of residential areas of rifampicin resistant-TB cases: A first retrospective study from Mizoram, Northeast India. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases 29: 100342.