In today’s modern world, the human race is losing the arm race with antibiotics. Ubiquitous bacterial pathogens have been continuously evolving to resist antibiotics. Hospitals, particularly intensive care units, are an important breeding ground for antibiotic-resistant bacteria because of factors like – over the counter antibiotic use, patient overcrowding, fraudulent infection control practices and use of excessive invasive devices, especially in developing countries (Mehrad et al., 2015). Such resistance raises the morbidity and mortality associated with infections and raises costs of prolonged healthcare, and the need for more upscale drugs (Cohen et al., 1992). India is one of the largest consumers of antibiotics. With widespread use of such broad-spectrum agents, the spread of multidrug resistant organisms (MRDO) has increased in both community and hospital settings (Laxminarayan et al., 2016, Teerawattanapong et al., 2018). In 2018, Gandra et al., analysed data on 5103 Patient-level antimicrobial susceptibility test results from 10 hospitals all over India (Gandra et al., 2018); the overall mortality rate of patients was 13.1% and there was a significant relationship between MDR and mortality. Infections with MDR and extensively drug resistant (XDR) E. coli, XDR K. pneumoniae, and MDR A. baumannii were associated with 2–3 times higher mortality. Such cases emphasise the importance of developing means to tackle the newly evolving resistant pathogens. In June 2017, the “EU One Health action plan against antimicrobial resistance” was adopted by the European Commission with a framework for reducing antimicrobial resistance as well as enhancing the development of new effective antimicrobials. Given the high attrition rates, substantial costs and slow pace of new drug discovery, we are urgently in need of an alternative method to fight bacterial infections. In such situations, use of bacteriophages, i.e. viruses that infect and kill bacteria, appears to be a promising alternative.
Bacteriophages: History
Ernest Hankin, a British bacteriologist first reported (Hankin, 1896) the presence of marked antibacterial activity against Vibrio cholerae in the waters of the Ganges and Yamuna rivers in India. He reported that an unidentified heat labile substance filterable through fine porcelain filters was responsible for this phenomenon. Two years later, the same phenomenon was observed by the Russian bacteriologist Gamaleya while working with Bacillus subtilis (Samsygina et al., 1984). In 1915 Frederick Twort, an English medically trained bacteriologist, reintroduced the subject by reporting a similar phenomenon and hypothesised that it may have been due to a virus (Twort, 1936). In 1917, Felix d’Herelle, a French-Canadian microbiologist at the Institut Pasteur in Paris, “officially” discovered bacteriophages. This rediscovery by d’Herelle is associated with an outbreak of severe hemorrhagic dysentery among French troops stationed at Maisons-Laffitte (on the outskirts of Paris) in July-August, 1915. While investigating the outbreak, d’Herelle made bacterium-free filtrates of the patients’ faecal samples and incubated them with Shigella strains isolated from the patients. On spreading these mixtures on agar cultures, he observed the appearance of small, clear areas, which he initially called taches, then taches vierges, and later, plaques (Summers et al., 1999). D’Herelle’s findings were presented and published during the September, 1917 meeting of the Academy of Sciences. d’Herelle strongly proposed that the phenomenon was caused by a virus capable of parasitizing bacteria and named it “bacteriophage” together with his wife Marie on 18 October, 1916. D’Hérelle reported that the phage always appeared in the stools of Shigella dysentery patients shortly before they began to recover. In the following years, phages were employed to treat dysentery and cholera with success. In 1919, studies were conducted at the Hôpital des Enfants-Malades in Paris under the clinical supervision of the hospital’s Chief of Pediatrics, Professor Victor-Henri Hutinel. To confirm the safety of the antidysentery phage preparation, it was ingested by d’Herelle, Hutinel and several hospital interns before administering it the next day to a 12-year-old boy with severe dysentery. The patient’s symptoms ceased after a single administration and the boy fully recovered within a few days. In 1921, Richard Bruynoghe and Joseph Maisin used bacteriophages to treat staphylococcal skin infections (BBruynoghe et al., 1921).
Bacteriophages: Commercial production
d’Herelle’s commercial laboratory in Paris, introduced the first commercial production of bacteriophages in the name: Bacté-coli-phage, Bacté-rhino-phage, Bacté-intesti-phage, Bacté-pyo-phage, and Bacté-staphy-phage, and they were marketed by what later became the large French company L’Oréal (Twort, 1936). In the 1940s, therapeutic phages against staphylococci, streptococci, Escherichia coli and other bacterial pathogens were introduced in the United States by the Eli Lilly Company (Indianapolis, Ind.). However, the efficacy of phage preparations was controversial (Kochetkova et al., 1989) and with the advent of antibiotics, commercial production of therapeutic phages ceased in most of the Western world. Nevertheless, in Eastern Europe and in the former Soviet Union, phages continued to be used therapeutically. Such activities were mainly conducted at the Eliava Institute of Bacteriophage, Microbiology and Virology (EIBMV) of the Georgian Academy of Sciences, Tbilisi, Georgia and the Hirszfeld Institute of Immunology and Experimental Therapy (HIIET) of the Polish Academy of Sciences, Wroclaw, Poland. The Eliava Institute was founded in 1923 by Giorgi Eliava, a prominent Georgian bacteriologist, together with Felix d’Herelle.
Bacteriophages: Prophylaxis and treatment
Successful implementation of the phage therapy was made during the Winter War between the former Soviet Union and Finland (1939–1940), when 6,000 Soviet soldiers were treated against open wounds with streptococcal or staphylococcal infections (Kiknadze et al., 1986). The wounds were topically treated, for example, with mixtures of streptococcal and staphylococcal phages or with pyophage (“PYO”) cocktail that contains phages to a wide variety of bacteria including streptococci, staphylococci, Shigella, Salmonella, Escherichia coli, Pseudomonas aeruginosa and Proteus (Kochetkova et al., 1989). During 1981-1986, Slopek et al. described the effectiveness of phages against infections caused by several bacterial pathogens including multidrug-resistant mutants (Slopek et al., 1987). They applied bacteriophage therapy in 550 cases of suppurative bacterial infections, in patients ranging in age from 1 week to 86 years. Positive results and transient improvements were obtained in 92.4% and 6.9% cases; whereas in 0.7% cases, the phage treatment proved to be ineffective. Considering that majority of patients (518 cases, 94.2%) were resistant to antibiotic treatment, the results of phage therapy was regarded favourable. During 1963 and 1964, extensive studies evaluating the utility of therapeutic phages for prophylaxis of infectious diseases was conducted in Tbilisi, Georgia (Babalova et al., 1968). A total of 30,769 children (6 months to 7 years old) suffering from bacterial dysentery were included in the study. Based on clinical diagnosis, the incidence of dysentery was 3.8-fold higher in the placebo group than in the phage-treated group (6.7 and 1.76 per 1,000 children, respectively) during the 109-day study period. Besides, phages have also been reported to be effective in treating staphylococcal lung infections (Meladze et al., 1982), P. aeruginosa infections in cystic fibrosis patients (Law et al., 2019), eye infections (Proskurov, 1970), neonatal sepsis (Pavlenishvili et al., 1993), urinary tract infections (Perepanova et al., 1995), and surgical wound infections (Peremitina et al., 1981), cerebrospinal meningitis in a newborn (Stroj et al., 1999), skin infections caused by Pseudomonas, Staphylococcus, Klebsiella, Proteus and E. coli (Cislo et al., 1987), recurrent subphrenic and subhepatic abscesses (Kwarcinski et al., 1994), and various chronic bacterial diseases (Kaczkowski et al., 1990). Phage therapy has also been reported to normalize tumour necrosis factor alpha (TNF-a) levels in serum and the production of TNF-a and interleukin-6 by blood cell cultures (Weber-Dabrowska et al., 2000). Zhukov-Verezhnikov et al. (1978) found that “adapted” bacteriophages (i.e., phages selected against bacterial strains isolated from individual patients) were five- to six fold more effective in curing suppurative surgical infections than were the commercially available preparations, presumably because of their improved specificity. Phages have also been related to the age old practise of faecal microbiota transplantation (FMT) that dates back to the China of the 4th century, where stool diluted with water and perhaps fermented, called “yellow soup”, was used against food poisoning and diarrhoea (Zhang et al., 2017). FMT has gained acceptance within the medical community to be effective against C. difficile infection, inflammatory bowel disease (IBD), obesity, possibly even mental disorders and others (Moelling et al., 2016).
In 2013, the European Commission started a therapeutic trial under the 7th Framework Program called PhagoBurn comprising eleven clinical EU partners from France, Belgium and Switzerland aimed at treating P. aeruginosa infected burn wounds with Good Manufacturing Practice (GMP) (Jault et al., 2018). As part of this trial, first commercial GMP-like production of phages was achieved by the French company Clean Cells. The most striking and well-documented case of phage therapy against superbug multidrug-resistant Acinetobacter baumannii strain was reported in 2017. Tom Patterson, who was infected with a multidrug-resistant Acinetobacter baumannii strain during a trip to Egypt, was treated with about 100 phages isolated from sewage water and environmental samples and screened for lytic activity against the patient’s A. baumannii strain. After being in coma for three months, the treatment was well tolerated and the patient recovered (Schooley et al., 2017). The phage preparations used were from the US Navy phage library at Texas A&M University, and one from AmpliPhi Biosciences, CA. Strathdee, Patterson’s wife together with Robert Schooley, University of California’s Center on Innovative Phage Applications and Therapeutics (IPATH) San Diego, CA wrote a book on how phage therapy saved her husband from a deadly superbug (to be published in 2019).
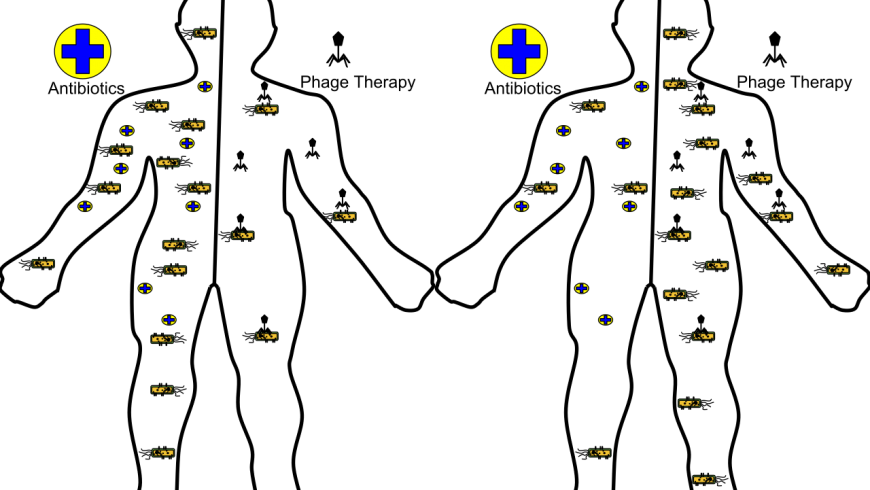
In another study, contamination with pan-resistant P. aeruginosa was reduced by surgeons of the German Military Hospital, Berlin, while treating a war-injured patient with a mixture of phages from the Eliava Institute, antibiotics and other detoxifying agents. The authors stressed the importance of combining phages with antibiotics and discussed about antimicrobial peptides or photodynamic therapies in combination with phages (Vogt et al., 2017). Phages may increase the uptake of antibiotics into bacterial cells. Therefore, phage therapy is likely most effective when combined with antibiotics (Vogt et al., 2017; Chaudhry et al., 2017). Jean-Paul Pirnay from the Queen Astrid Military Hospital in Brussels, Belgium, also advocates of benefits of phage therapy and published a proposal for guidelines on implementation of phage therapy (Pirnay et al., 2018).
Phage therapy was also advocated in the work of Elizabeth Kutter in the treatment of diabetic foot ulcers that are often infected with MRSA strains or other multidrug resistant bacteria. Kutter found that patients with MRSA infection and poor response to antibiotics could be successfully treated topically with a staphylococcal phage (Fish et al., 2016). Furthermore, phage therapy was also successful against the second most frequently implicated bacterium in diabetic foot infections, Klebsiella pneumoniae (Taha et al., 2018).
Bacteriophages: advantages over antibiotics
Lytic phages are similar to antibiotics but have some at least theoretical advantages over antibiotics and have been reported to be more effective in treating infections in humans and experimentally infected animals. Antibiotics are revolutionized medicines that kill bacteria by disrupting one or more of the important processes that bacteria need to survive. Because these are common processes, one “broad spectrum” antibiotic could potentially kill many species of bacteria at once. While antibiotics are often very effective in stopping bacterial infections, well-developed phages could have several advantages over antibiotics. First, phages are specific to one species of bacteria and are therefore unlikely to disturb beneficial microbes living in our body. Because phages kill with a narrow scope, therefore, dysbiosis and chances of developing secondary infections are avoided (Chernomordik et al., 1989). Second, antibiotics are metabolized and eliminated from the body and do not necessarily concentrate at the site of infection. However, phages have “exponential growth” at the site of infection and thus may require less frequent phage administration in order to achieve the optimal therapeutic effect (Smith et al., 1982).
Third, multiple side effects, including intestinal disorders, allergies and secondary infections (e.g. yeast infections) have been reported on use of antibiotics. On the other hand, only a few minor side effects reported (Stroj et al., 1999; Cislo et al., 1987) for therapeutic phages due to the liberation of endotoxins from bacteria lysed in vivo by the phages.
Fourth, resistance to antibiotics is not limited to targeted bacteria but phage-resistant bacteria remain susceptible to other phages having a similar target range (Salyers et al., 1997). Fifth, developing a new antibiotic (e.g. against antibiotic-resistant bacteria) is a time-consuming process (Silver et al., 1993). Selecting new phages (e.g. against phage-resistant bacteria) is a relatively rapid process and evolutionary arguments have supported the idea that active phages can be selected against every antibiotic-resistant or phage-resistant bacterium by the process of natural selection.
Why aren’t phages used?
From a clinical standpoint, phages appear to be innocuous. During the long history of using phages as therapeutic agents in Eastern Europe and the former Soviet Union, phages have been administered to humans as (i) oral tablet or liquid formulations, (ii) rectal inoculation, (iii) local applications (skin, eye, ear, nasal mucosa, etc.), (iv) as aerosols or intrapleural injections, and (v) intravenously. There have been virtually no reports of serious complications associated with their use. However, it would be prudent to ensure further the safety of therapeutic phages before widely using them as therapeutic agents.
First, because of the high specificity of phages, many negative results may have been obtained because of the failure to select lytic phages for the targeted bacterial species (D’Herelle et al., 1930). Second, phages are more difficult to prepare cleanly. Early therapeutic phages were in crude lysates of host bacteria, and they contained numerous contaminants (including endotoxins) that may have counteracted the effect of phage and trigger a deadly immune response called sepsis in the host body. Obtaining the right concentration of phages is another challenge. At low concentrations, phage therapy would be inefficacious. Third, there are problems of poor stability and viability of phage preparations. Some commercial phage preparations were supplemented with mercurials or oxidizing agents or were heat-treated to ensure bacterial sterility (Carlton et al., 1999) but instead these treatments may have inactivated the phages. Fourth, there is a problem related to lack of understanding to differentiate between lytic and lysogenic phages, which are heterogenous and have different mode of action. Fifth, phage takes a longer time to employ in a treatment compared to antibiotics. Because of narrow host range, phage selection has to be done with care. Proper diagnosis of the pathogen is must for success of the therapy and is tedious. Sixth, most clinical studies using therapeutic phages were conducted without placebo controls and thus lack scientific credibility (Eaton et al., 1934; Krueger et al., 1941).
Conclusion
Given the immense potential that bacteriophages hold, it is important to accelerate the availability of phage therapy. Phages have been proven beneficial in limiting the rise in antibiotic resistance associated with agricultural and livestock farming practices. Indeed, three different phage-based products (Agriphage in the US, Erwiphage in Hungary and Biolyse in the UK), successful against bacterial crop diseases, are currently in the market (Buttimer et al., 2017). Furthermore, the phage therapy has also been used against zoonotic and infectious diseases in livestock farming and aquaculture (Atterbury et al., 2009; Richards et al., 2014; Doss et al., 2017). Bacteriophages have also been used for development of surface sanitizers and are commercialised by two US companies against Salmonella (BacWash™) and E. coli O157:H7 (Finalyse™) (Hernández et al., 2011). Bacteriophage application as food bio-preservatives has received GRAS designation by the FDA and currently marketed in the US against Listeria monocytogenes (Listshield™), Salmonella enteric (SalmoFresh™) and Escherichia coli (Ecoshield™) (Fernández et al., 2018). Use of bacteriophages has also been implicated in development of bacterial diagnosis (O’Sullivan et al., 2016). Phage receptor-binding proteins (RBPs) have also been used successfully in Campylobacter phage NCTC12673 to create a simple glass slide agglutination test for Campylobacter. The RBP, when fused to green fluorescent protein, allowed the detection of C. jejuni and C. coli isolates through fluorescent microscopy (Javed et al., 2013). With the advent of phage display, first described in 1985 by Smith (Smith et al., 1985), numerous applications in the identification of receptor and ligand interactions were postulated leading to drug discovery (Omidfar et al., 2015) and vaccine design (Gao et al., 2010). Furthermore, bacteriophages have found their application in development of monoclonal antibodies (Shukra et al., 2014).
Thus, efforts should be made to develop interim regulations by authorities with reduced stringency on the use of bacteriophages. Information on phage banks should become available to physicians and researchers. Large phage collections already exist in Brussels, Belgium, Tbilisi, Republic of Georgia, Novosibirsk, Russia, Braunschweig, Germany, Zurich, Switzerland, Helsinki, Finland, and Quebec City, Canada but are not easily accessible. The preparation of phages “in the spirit of GMP” should be performed with the help of magisterial preparations by pharmacies as recommended. It should be kept in mind that phage therapy is a promising adjunct to humankind and their knowledge must be used judiciously for betterment of mankind.
References
Atterbury R. J. (2009). Bacteriophage biocontrol in animals and meat products. Microb. Biotechnol. 2, 601–612. 10.1111/j.1751-7915.2009.00089.
- Bruynoghe, R., and J. Maisin. (1921). Essais de the ´rapeutique au moyen du bacteriophage. C. R. Soc. Biol. 85:1120–1121
Babalova, E. G., K. T. Katsitadze, L. A. Sakvarelidze, N. S. Imnaishvili, T. G. Sharashidze, V. A. Badashvili, G. P. Kiknadze, A. N. Meipariani, N. D. Gendzekhadze, E. V. Machavariani, K. L. Gogoberidze, E. I. Gozalov, andN. G. Dekanosidze. (1968). Preventive value of dried dysentery bacteriophage.Zh. Mikrobiol. Epidemiol. Immunobiol. 2:143–145.
Buttimer C., McAuliffe O., Ross R. P., Hill C., O’Mahony J., Coffey A. (2017). Bacteriophages and bacterial plant diseases. Front. Microbiol. 8:34. 10.3389/fmicb.2017.00034
Carlton, R. M. 1999. Phage therapy: past history and future prospects. Arch.Immunol. Ther. Exp. 5:267–274
Chaudhry W.N., Concepción-Acevedo J., Park T., Andleeb S., Bull J.J., Levin B.R. Synergy and order effects of antibiotics and phages in killing Pseudomonas aeruginosa biofilms. PLoS ONE. 2017;12:e0168615. doi: 10.1371/journal.pone.0168615.
Chernomordik, A. B. 1989. Bacteriophages and their therapeutic-prophylactic use. Med. Sestra 6:44–47
Cislo, M., M. Dabrowski, B. Weber-Dabrowska, and A. Woyton. (1987). Bacteriophage treatment of suppurative skin infections. Arch. Immunol. Ther.
Exp. 2:175–183.
Cohen, M.L. (1992). Epidemiology of drug resistance: implications for a post-antimicrobial era. Science. 257(5073):1050-5
D’Herelle, F. 1930. The bacteriophage and its clinical applications. Charles C Thomas, Springfield, Ill
Doss J., Culbertson K., Hahn D., Camacho J., Barekzi N. (2017). A review of phage therapy against bacterial pathogens of aquatic and terrestrial organisms. Viruses 9:E50. 10.3390/v9030050
Eaton, M. D., and S. Bayne-Jones. 1934. Bacteriophage therapy. Review of the principles and results of the use of bacteriophage in the treatment of infections. JAMA 23:1769–1939
Fernández, Lucía et al. “Application of Bacteriophages in the Agro-Food Sector: A Long Way Toward Approval.” Frontiers in cellular and infection microbiology vol. 8 296. 22 Aug. 2018, doi:10.3389/fcimb.2018.00296
Fish R., Kutter E., Wheat G., Blasdel B., Kutateladze M., Kuhl S. Bacteriophage treatment of intransigent diabetic toe ulcers: A case series. J. Wound Care. 2016;25:273. doi: 10.12968/jowc.2016.25.Sup7.S27.
Gandra, S., Tseng, k.K., Arora, A., Bhowmik, B., Robinson, M.L., Panigrahi, B., Laxminarayan, R., Klein, E.Y. (2018). The mortality burden of multidrug resistant pathogens in India: a retrospective observational study. Clin Infect Dis.
Gao J, Wang Y, Liu Z, et al. : Phage display and its application in vaccine design. Ann Microbiol. 2010;60(1):13–9. 10.1007/s13213-009-0014-7
Hankin E.H. (1896). L’action bactericide des eaux de la Jumna et du Gange sur le vibrion du cholera (in French) Ann. Inst. Pasteur. 10: 511–523.
Hernández A., Ruiz F. M., Romero A., Martínez J. L. (2011). The binding of triclosan to SmeT, the repressor of the multidrug efflux pump SmeDEF, induces antibiotic resistance in Stenotrophomonas maltophilia. PLoS Pathog. 7:e1002103.
Jault P., Leclerc T., Jennes S., Pirnay J.P., Que Y.A., Resch G., Rousseau A.F., Ravat F., Carsin H., Le Floch R., et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. Lancet Infect. Dis. 2018 doi: 10.1016/S1473-3099(18)30482-1.
Javed MA, Poshtiban S, Arutyunov D, et al. : Bacteriophage receptor binding protein based assays for the simultaneous detection of Campylobacter jejuni and Campylobacter coli. PLoS One. 2013;8(7):e69770. 10.1371/journal.pone.0069770
Kaczkowski, H., B. Weber-Dabrowska, M. Dabrowski, Z. Zdrojewicz, and F.Cwioro. (1990). Use of bacteriophages in the treatment of chronic bacterial diseases. Wiad. Lek. 43:136–141.
Kiknadze, G. P., M. M. Gadua, E. V. Tsereteli, L. S. Mchedlidze, and T. V.Birkadze. (1986). Efficiency of preventive treatment by phage preparations of children’s hospital salmonellosis, p. 41–44. In G. P. Kiknadze (ed.), Intestinal infections. Sovetskaya Meditsina, Tbilisi, Georgia.
Kochetkova, V. A., A. S. Mamontov, R. L. Moskovtseva, E. I. Erastova, E. I. Trofimov, M. I. Popov, and S. K. Dzhubalieva. (1989). Phagotherapy of postoperative suppurative-inflammatory complications in patients with neoplasms. Sov. Med. 6:23–26
Krueger, A. P., and E. J. Scribner. 1941. Bacteriophage therapy. II. The bacteriophage: its nature and its therapeutic use. JAMA 19:2160–2277
Kwarcinski, W., B. Lazarkiewicz, B. Weber-Dabrowska, J. Rudnicki, K.Kaminski, and M. Sciebura. (1994). Bacteriophage therapy in the treatment of recurrent subphrenic and subhepatic abscess with jejunal fistula after stomach resection. Pol. Tyg. Lek. 49:535
Law, N., Logan, C., Yung, G., Furr, C.L., Lehman, S.M., Morales, S., Rosas, F., Gaidamaka, A., Bilinsky, I., Grint, P., Scgooley, R.T., Aslam, S. (2019). Successful adjunctive use of bacteriophage therapy for treatment of multidrug resistant Pseudomonas aeruginosa infection in cystic fibrosis patient. Infectioin. 47(4): 665-668.
Laxminarayan, R., Chaudhury, R.R. (2016). Antibiotic resistance in India: Drivers and opportunities for action. PLoS Med. 13(3)
Mehrad, B., Clark, N.M., Zhanel, G.G., Lynch J.P. (2015). Antimicrobial resistance in hospital-acquired gram negative bacterial infection. Chest. 147(85):1413-1421
Meladze, G. D., M. G. Mebuke, N. S. Chkhetia, N. I. Kiknadze, G. G.Koguashvili, I. I. Timoshuk, N. G. Larionova, and G. K. Vasadze. (1982). The efficacy of staphylococcal bacteriophage in treatment of purulent diseases of lungs and pleura. Grudn. Khir. 1:53–56
Moelling, K., Broecker, F. 2016. Fecal microbiota transplantation to fight Clostridium difficle infections and other intestinal diseases. Bacteriophage. 6(4)
Omidfar K, Daneshpour M: Advances in phage display technology for drug discovery.Expert Opin Drug Discov. 2015;10(6):651–69. 10.1517/17460441.2015.1037738
O’Sullivan, Lisa et al. “Bacteriophage-based tools: recent advances and novel applications.” F1000Research vol. 5 2782. 29 Nov. 2016, doi:10.12688/f1000research.9705.1
Pavlenishvili, I., and T. Tsertsvadze. (1993). Bacteriophagotherapy and enterosorbtion in treatment of sepsis of newborns caused by gram-negative bacteria. Pren. Neon. Infect. 11: 104.
Peremitina, L.D., Berillo, E.A., Khvoles, A.G. (1981). Experience in the therapeutics use of bacteriophage preparation in suppurative surgical infections. Zh Mikrobiol Epidemiol Immunobiol. (9):109-10
Perepanova, T.S., Darbeeva, O.S., Kotliarova, G.A., Kondrat’eva, E.M., Maiskaia, L.M., Malysheva, V.F., Baiguzina, F.A., Grishkova, N.V. (1995). The efficiency of bacteriophage preparations in treating inflammatory urologic diseases. Urol Nefrol (Mosk). (5):14-7
Pirnay J.P., Verbeken G., Ceyssens P.J., Huys I., de Vos D., Ameloot C., Fauconnier A. The Magistral Phage. Viruses. 2018;10:64. doi: 10.3390/v10020064.
Proskurov, V.A. (1970). Use of staphylococcal bacteriophage for therapeutic and preventive purposes. Zh Mikrobiol Epidemiol Immunobiol. 47(2): 104-7
Richards G. P. (2014). Bacteriophage remediation of bacterial pathogens in aquaculture: a review of the biotechnology. Bacteriophage 4:e975540 10.4161/21597081.2014.975540
Salyers, A. A., and C. F. Amabile-Cuevas. 1997. Why are antibiotic resistance
genes so resistant to elimination? Antimicrob. Agents Chemother. 41:2321–2325.
Samsygina, G.A., Boni, E.G. (1984). Bacteriophage and phage therapy in pediactric practice. Pediatriia. (4):67-70
Schooley R.T., Biswas B., Gill J.J., Hernandez-Morales A., Lancaster J., Lessor L., Barr J.J., Reed S.L., Rohwer F., Benler S., et al. Development and Use of Personalized Bacteriophage-Based Therapeutic Cocktails to Treat a Patient with a Disseminated Resistant Acinetobacter baumannii Infection. Antimicrob. Agents Chemother. 2017;61:e00954-17. doi: 10.1128/AAC.00954-17.
Shukra, A M et al. “Production of recombinant antibodies using bacteriophages.” European journal of microbiology & immunology vol. 4,2 (2014): 91-8. doi:10.1556/EuJMI.4.2014.2.1
Silver, L. L., and K. A. Bostian. 1993. Discovery and development of new antibiotics: the problem of antibiotic resistance. Antimicrob. Agents Chemother. 37:377–383
Slopek, S., B. Weber-Dabrowska, M. Dabrowski, and A. Kucharewicz Krukowska. (1987). Results of bacteriophage treatment of suppurative bacterial infections in the years 1981–1986. Arch. Immunol. Ther. Exp. 35:569–583.
Smith GP: Filamentous fusion phage: novel expression vectors that display cloned antigens on the virion surface. Science. 1985;228(4705):1315–7. 10.1126/science.4001944
Smith, H. W., and M. B. Huggins. 1982. Successful treatment of experimental Escherichia coli infections in mice using phages: its general superiority over antibiotics. J. Gen. Microbiol. 128:307–318.
Stroj, L., B. Weber-Dabrowska, K. Partyka, M. Mulczyk, and M. Wojcik. (1999). Successful treatment with bacteriophage in purulent cerebrospinal meningitis in a newborn. Neurol. Neurochir. Pol. 3: 693–698.
Summers, W. C. (1999). Felix d’Herelle and the origins of molecular biology. Yale University Press, New Haven, Conn
Taha O.A., Connerton P.L., Connerton I.F., El-Shibiny A. Bacteriophage ZCKP1: A potential treatment for Klebsiella pneumoniae isolated from diabetic foot patients. Front. Microbiol. 2018;9:2127. doi: 10.3389/fmicb.2018.02127.
Teerawattanapong, N., Panchi, P., Kulpokin, D., Na Ranong, S., Kongpakwattana, K., Saksinanon, A., Goh, B.H., Lee, L.H., Apisarnthanarak, A., Chaiyakunapruk, N. (2018). A systemic review of the burden of multidrug resistance healthcare associated infections among intensive care unit patients in Southeast Asia: The rise of multidrug resistant Acinetobacter baumannii. Infect Control Hosp Epidemiol. 39(5):525-533
Twort, F.W. (1936). Further investigations on the nature of ultramicroscopic viruses and their cultivation. J Hyg (Lond). 36(2):204-35.
Vogt D., Sperling S., Tkhilaishvili T., Trampuz A., Pirnay J.P., Willy C. “Beyond antibiotic therapy”—Zukünftige antiinfektiöse Strategien—Update 2017 (in German) Unfallchirurg. 2017;120:573–584. doi: 10.1007/s00113-017-0374-6.
Weber-Dabrowska, B., M. Zimecki, and M. Mulczyk. (2000). Effective phage therapy is associated with normalization of cytokine production by blood cell cultures. Arch. Immunol. Ther. Exp. 48:31–37
Zhang, F., Luo, W., Shi, Y., Fan, Z., Ji, G. 2012. Should we standardize the 1700 year old fecal microbiota transplantation? Am j Gastroenterol. 107(11):1755
Zhukov-Verezhnikov, N. N., L. D. Peremitina, E. A. Berillo, V. P. Komissarov, V. M. Bardymov, A. G. Khvoles, and L. B. Ugryumov. 1978. A study of the therapeutic effect of bacteriophage agents in a complex treatment of suppurative surgical diseases. Sov. Med. 12:64–66.
Author information Name of the Author/Authors: Moushumee Das and Pankaj Deka Designation of Author/Authors: Junior Research Fellow at the Department of Microbiology, CVSc, AAU, Khanapara Asst. Professor, Department of Microbiology, CVSc, AAU, Khanapara E-mail ID of Author/Authors: moushumee88@gmail.com, drpankajaau@gmail.com Name and address of the Institute to which the Author/Authors are associated: Department of Microbiology, College of Veterinary Sciences, AAU, Khanapara, Guwahati, Assam, PIN-781022