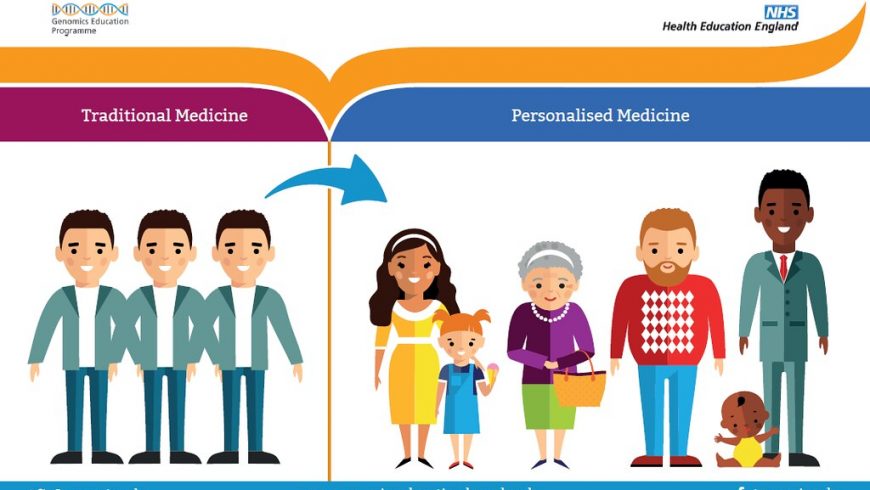
Personalized medicine is a form of medicine that uses information about a person’s genes, proteins, and environment in order to prevent, diagnose and treat diseases. Specific information about a person’s tumor may be used in personalized medicine to help diagnose a cancer, plan treatment, find out the efficacy of treatment, or make a prognosis. Examples of this form of medicine include application of targeted therapies to treat specific types of cancer cells, or using a test for detection of tumor markers to help diagnose cancer.
Historical background:
The term personalized medicine first appeared in published works in 1999, however some of the field’s core concepts have been in existence since the early 1960s (Jain, 2002). Personalized medicine has been now made a more tangible reality by the advent of new technologies. It has enabled researchers to provide a link between the molecular and the clinical profiles of an individual. Two key discoveries have allowed for significant progress within the field of personalized medicine – single nucleotide polymorphism (SNP) genotyping and microarray/biochips. SNPs are single nucleotide changes in the DNA sequence that are particularly frequent in the population, and account for 90% of all known polymorphisms (Bernardini, 2010; Jain, 2002). The ability to identify these polymorphisms is crucial, as SNPs have been linked to the susceptibility of the patient to various disease processes and responsiveness to therapy. SNPs have also been proved to be an invaluable tool to segregate patients in a multitude of studies and clinical trials.
The invention of the microarray biochip has revolutionized the field of personalized medicine, specifically by creating the ability to store and rapidly analyze a patient’s genome sequence. Biochip technology enables researchers and clinicians to do SNP genotyping efficiently and thereby allowing rapid development of protein-based diagnostics and therapeutics.
Example of Personalized medicine:
Abacavir, a nucleotide reverse transcriptase inhibitor used to treat patients with HIV, is known to cause a hypersensitivity reaction in some patients within six weeks of the onset of therapy. Before the advent of personalized medicine, this hypersensitivity reaction was detected based on clinical symptoms. In 2002, two independent studies demonstrated a possible genetic link between the hypersensitivity reaction and the major histocompatibility complex (MHC) class I allele HLA-B*57:01. Mallal et al. (2002) conducted a follow up study in which they gave abacavir only to patients who were negative for the HLA-B*57:01 gene, and there was no hypersensitivity reaction in that patient population. The results demonstrated that patients that carry the HLA-B*57:01 gene have a 60% chance of developing a hypersensitivity reaction when treated with abacavir, while patients who do not carry the gene do not develop the drug reaction at all. This landmark study demonstrated that a patient’s genome can predict response to a specific drug therapy. Moreover, results of this study was so convincing that the Food and Drug Administration and the European Medicines Agency altered the abacavir label to advise testing for the HLA-B*57:01 allele prior to using abacavir to treat HIV (Bernardini, 2010).
Besides preventing adverse reactions, personalized medicine can assist clinicians in determining ideal drug dosing for their patients. For instance, warfarin, a vitamin K antagonist, is commonly used as a blood thinner. Warfarin has a narrow therapeutic range, and supratherapeutic dosages place the patient at an increased risk for adverse bleeding, while subtherapeutic levels leave the patient prone to clotting. Usually a patient’s dose response to warfarin can hardly be predicted by the typical patient attributes and the therapy is initiated with substantial risk. Personalized medicine has recently begun to explain this variable patient response. Studies have shown that variation in three genes can explain some of the inter-individual variability of this drug. These three genes are: CYP2C9 that encodes the enzyme responsible for warfarin metabolism; VKORC1 that encodes the enzyme that recycles vitamin K, the primary target of the drug, and CYP4F2 that encodes the enzyme responsible for vitamin K metabolism (Bernardini, 2010). Borgiani et al. (2009) previously demonstrated that variants of these three genes along with age and weight of the patient can explain 60.5% of the dosing variability among patients. The quest of personalized medicine to improve warfarin dosing has led to changes in the FDA label to include consideration of genetic variations in drug initiation, and has catalyzed the development of genetic tests that enable clinicians to initiate warfarin treatment more accurately.
Finally, personalized medicine can help predict a patient’s likelihood of developing certain illnesses. Well-known examples are mutations of BRCA1 and BRCA2 genes that have been implicated in familial breast cancers and the loss of APC gene function in familial adenomatous polyposis. As advancements in personalized medicine continue, clinicians continue to gain new tools to help identify patients at risk for developing a debilitating disease. One such disease is age-related macular degeneration (AMD), one of the most common causes of visual impairment in adults over 50 years of age. The recent discovery of two genes, CFH and ARMS2, which have a strong association with the development of AMD, may allow for development of genetic tests that help physicians to identify the patients at risk (Bernardini, 2010).
Future of personalized medicine:
Human genome research is the foundation for the future of personalized medicine, and has the ability to eventually customize medical treatments to individual patients through the incorporation of genetics, molecular profiles and clinical characteristics in deciding appropriate treatment regime. With the use of risk algorithms, molecular diagnostics and targeted therapies, the field of personalized medicine is striving to translate research into clinical practice. Advances within personalized medicine will also increase the efficiency and pace of pharmaceutical development in the near future, as drug developers can now use toxigenomic markers to screen compounds and improve selection of patients for clinical trials to reduce the number of failures in later stages of drug development. Further, toxigenomic markers predictive of adverse drug reactions can be used to prevent patients from receiving therapy that will harm rather than cure.
One of the most promising areas within personalized medicine is pharmacogenetics, which evaluates influence of patient’s genetic makeup on treatment efficacy. Researchers within this field are focused on developing the “Dx-Rx paradigm” which requires genetic/biomarker testing before prescription writing. However, use of this paradigm in treating diseases requires understanding the value in genetic and molecular diagnostics to manage the use of costly therapies. Consequently, researchers need to develop diagnostic tests that can accurately identify responders from non-responders to a specific treatment. In spite of the proven clinical benefit of personalized medicine, further research is needed to elucidate the effect of this field on cost of therapy and its outcome (i.e., morbidity and mortality) and the overall societal benefit.
References:
Bernardini, L.; Alesi, V.; Loddo, S.; Novelli, A.; Bottillo, I.; Battaglia, A.; Digilio, M.C.; Zampino, G.; Ertel, A.; Fortina, P. and Surrey, S. (2010). High-resolution SNP arrays in mental retardation diagnostics: how much do we gain? European Journal of Human Genetics, 18(2): 178.
Ferrara, J. (2007). Personalized medicine: challenging pharmaceutical and diagnostic company business models. McGill Journal of Medicine, 10(1): 59.
Jain, K.K. (2002). From Molecular Diagnostics to Personalized Medicine, Expert Review of Molecular Diagnostics, 2(4): 299-301, DOI: 10.1586/14737159.2.4.299.
Mallal, S.; Nolan, D.; Witt, C.; Masel, G.; Martin, A.M.; Moore, C.; Sayer, D.; Castley, A.; Mamotte, C.; Maxwell, D. and James, I. (2002). Association between presence of HLA-B* 5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. The Lancet, 359(9308): 727-732.
Author- Tridip Boruah, M.Phil Research Scholar, Department of Botany, Gauhati University, Guwahati-781014, Assam, India, Email- tridip_boruah@gauhati.ac.in Phone- 8876330933