Research Highlights
Unrevealing the genesis of “Omicron”
By the end of 2021, the world has understood the impact of COVID-19 in most of the dimensions of life; however, there are many mysteries in the genesis, virulence, pathogenesis, evolution and mutation of SARS-CoV-2. Since 2020, we are experiencing new heats of COVID-19 in terms of its variants. The recent SARS-CoV-2 novel variant (B.1.1.529) designated as variant of concern ‘Omicron’ got its identity in November, 2021. Initially it was reported from Africa but within a very short span of time it conquered the entire globe. Although it is dominant over the older variants, there are knowledge gaps in its origin and evolution. Therefore, to find the genesis of Omicron, a team of scientists evaluated almost 4200 complete genomes of SARS-CoV-2 available in the public domain using bioinformatics tools. It was observed that Omicron is a chimera, which is a result of recombination events between two lineages of SARS-CoV-2. The major parents of Omicron belongs to PANGO lineage (BA.1) of SARS-CoV-2 such as SARS-CoV-2/human/USA/COR-21-434196/2021 and strains like SARS-CoV-2/human/IRN/Ir-3/2019 belonging to B.35 that acted as minor parents. The recombination event between these two lineages resulted in substitution of 22 amino acids with 16 vital substitutions only in the spike protein. However, in another study it was observed that the mutations in the spike protein have shifted the tropism and fusogenicity of the Omicron variant. The replication efficiency of the Omicron variant is similar to the delta variant in the nasal epithelial cells of human; however, in lower airway like lung cells and gut cells, the replication efficiency is lower. Moreover, the spike protein of Omicron has more affinity for its receptor ACE2 than Delta. Thus, available vaccines and antiviral drugs such as remdesivir and molnupiravir retain their potency and efficiency for the Omicron variant of SARS-CoV-2.
Sources:
Oral mRNA vaccine is now not a dream
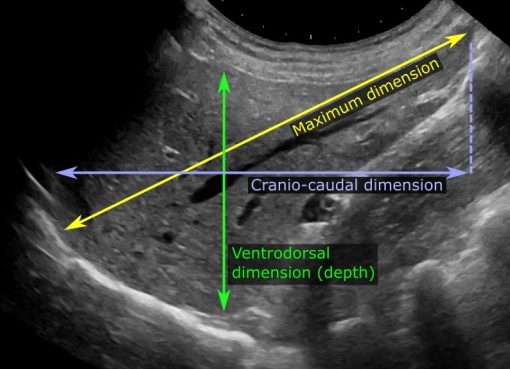
Nucleic acid based (DNA and RNA) therapeutics and prophylaxis have tremendous scope to treat and prevent diseases from cancer to COVID-19. However, the injectable formulation of DNA or RNA is a fear factor for many individuals as it causes pain, inflammation and fever in certain cases. Most of the people prefer oral medicines compared to injectable ones but one of the major constraints in formulating an oral-based nucleic acid vaccine or drug is the bioavailability, as the environment of gastrointestinal tracts degrades nucleic acid prior to its uptake by the target cells. Thus, researchers from multiple institutes of USA have designed ingestible milli-injector capsules of mRNA nanoparticles based on branched hybrid poly(β-amino ester). The formulated capsules could efficiently deliver mRNAs to different cells of gastrointestinal tract like gastric, delta, and parietal cells as well as there was systemic delivery. The formulation was validated in two animal models, rodents and pigs. Thus, the observations made in this study have opened the window for development of oral based mRNA vaccines or therapeutics in future.
Source: https://doi.org/10.1016/j.matt.2021.12.022
Another dark side of CRISPR-Cas9
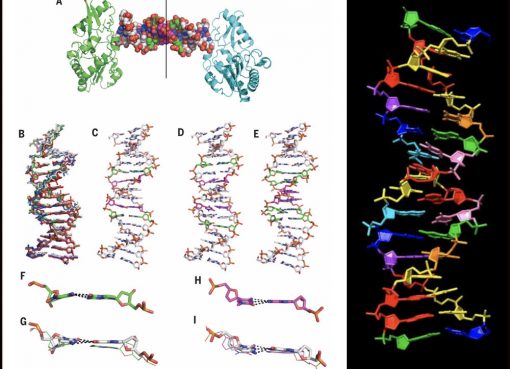
CRISPR-Cas9 is the most promising and popular genome editing tool in this era and it has revolutionized the field of biotechnology and biomedicine, particularly the treatment of genetic diseases. Although CRISPR-Cas9 technology has potential to cure genetic defects, the gene editing of human germline has many ethical constraints. Another controversy of CRISPR-Cas9 technology is the off-target mutations in the genome which could be fatal if such mutations disrupt the functions of vital gene(s). Before getting rid of the off-target mutations, CRISPR-Cas9 technology is suffering from another vital constraints, i.e. structural variants at on-target sites and off-target mutations could be inherited to the next generation. This constraint was tested in fertilized zebrafish eggs model and it was observed that both large structural variants at on-target sites and off-target mutations are inherited to the next generation in considerable percentage. Hence, before clinical use of CRISPR-Cas9 technology to treat genetic disorders, it is essential to ensure the safety of the protocol by pre-testing its off-target activity and structural variants in the patient material.
Source: https://doi.org/10.1038/s41467-022-28244-5
Pig: A potential organ donor for Homo sapiens
There is a huge shortage in human organ donors for transplantation across the globe. Moreover, to identify match organ donor is one more hurdle in organ transplantation. Therefore, many scientists have proposed the use of genetically modified animals to figure out the shortage of organ donors. Recently, there was a breakthrough in medical science when a human patient’s life was saved by heart transplantation which was received from a genetically engineered pig. In Maryland, a 57 years old patient, Mr. David Bennett, suffering from terminal heart disease was unable to find donor for his diseased heart and it was a do or die situation for him. However, as the last option for his survival, a skilful and eminent team of surgeons from University of Maryland Medical Center transplanted a heart from genetically manipulated pig after getting proper approval from competent authority and from the patient. The pig had 10 key genetic manipulations which included deletion of four genes and addition of six human genes to increase the compatibility with human physiological systems, particularly the immunological system. The transplantation operation was successful after eight hours of surgery which gave a new life to Mr. Bennett. This successful story has paved the rays of hope for many unfortunate patients who could not find organ donor(s) in the right time. Although, this is considered as the first successful transplant of a pig’s organ (heart) into human body (xenotransplant), the attempt is not new. Because about 25 years ago, in early 1997, the cardio-thoracic surgeon, Dr. Dhaniram Baruah from Assam, India transplanted pig’s organs into a human patient (Purno Saikia) with organ failure. However, it was considered unethical and unlawful at that point of time due to one or other reasons and the surgeon was put behind the bars. But the recent successful xenotransplantation for saving life of Mr. Bennett is a blessing to the humanity.
Sources:
- https://doi.org/10.1038/d41586-022-00111-9
- https://www.nytimes.com/2022/01/10/health/heart-transplant-pig-bennett.html
- Karmakar, R. (2022). A pig heart transplant in Assam in 1997. The Hindu. Accessed online on 6th February, 2022.