Dr. Manoj Kumar Kalita1, Dr. Himangshu Baruah2 and Dr. Prerona Patowary3
1Assistant Professor, Lakhimpur College of Veterinary Science, AAU, Joyhing, NLP-51
2Associate Professor, Lakhimpur College of Veterinary Science, AAU, Joyhing, NLP-51
3Scientist, AAU-Goat Research Station, Burnihat- 23
Introduction
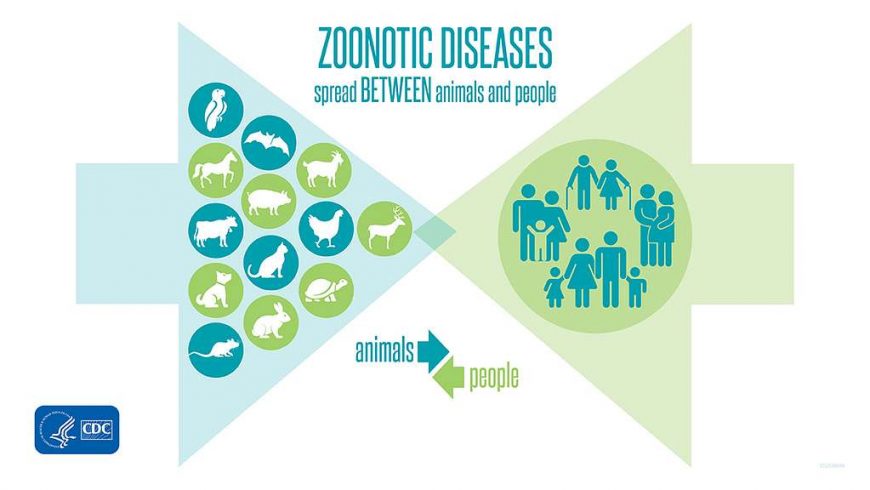
Zoonoses are infectious diseases transmitted between species, either from animals to humans or vice versa. Of the 1,461 recognized infectious diseases in humans, approximately 60% are caused by multi-host pathogens, which have the ability to spread across various species. Among these, 177 are classified as emerging or re-emerging zoonotic pathogens, which are twice as likely to fall into these categories compared to the non-zoonotic pathogens. The COVID-19 pandemic, caused by SARS-CoV-2 (a corona virus similar to the virus responsible for severe acute respiratory syndrome, SARS), is a striking example of the disruptive potential zoonotic agents can have on human life.
The transmission and emergence of zoonotic pathogens can occur through various means, including contact with companion animals (such as dogs, cats, or exotic pets), recreational activities (such as water sports, hunting, or the movement of animals for sporting purposes), globalization, tourism, livestock movement, and changes in land use or urbanization. The general public, including many pet owners, are often unaware that pets and other animals can harbour infectious agents transmissible to humans and are typically unfamiliar with methods for preventing zoonotic diseases.
Brucellosis
Brucellosis is a zoonotic disease of significant economic importance. Although it has been eradicated in regions like Europe, Australia, Canada, Israel, Japan, and New Zealand, it remains a persistent problem in areas of high endemicity, such as Africa, the Mediterranean, the Middle East, parts of Asia, and Latin America. Brucella species are small, nonmotile, aerobic, facultative intracellular, Gram-negative coccobacilli. All domestic species, except for cats, can be affected by brucellosis, and although horses are relatively resistant, they can still contract and transmit the disease to humans. Brucellosis in animals leads to considerable economic losses through decreased milk production, abortions, weak offspring, weight loss, infertility, and lameness. In severe cases, death may occur due to acute metritis following retained fetal membranes. Equine brucellosis often manifests as fistulous withers or poll evil.
Human brucellosis is typically an occupational disease, affecting those who work in close contact with infected animals, such as slaughterhouse workers, butchers, and veterinarians. Transmission occurs when infected animals or materials come into contact with skin abrasions. Human brucellosis can range from non-specific, flu-like symptoms to more severe conditions like undulant fever, arthritis, and orchiepididymitis in males. Chronic cases may result in fatigue, depression, and arthritis. Diagnosis is primarily based on serologic testing, as isolating B. abortus can be challenging. Prevention relies on early diagnosis, barrier precautions, and careful handling of laboratory materials. Molecular diagnostic tools, such as Light Cycler-based real-time PCR (LC-PCR), have been developed for rapid detection of Brucella DNA in serum samples.
In India, brucellosis is responsible for significant economic losses, estimated at Rs. 350 million annually in the form of lost food animals and labor. Human brucellosis contributes to the loss of 3 million man-days of labour each year. Infected animals show increased rates of abortion, stillbirth, infertility, calf mortality, and lameness, resulting in reduced milk production. Seroprevalence in India is reported at 22.18% by enzyme linked immunosorbent assay (ELISA), 13.78% by Rose Bengal plate test (RBPT), and 12.82% by milk ring test (MRT). Brucellosis is highly prevalent in regions like Togo, Mali, India, Sudan, and others.
Brucellosis primarily affects farmers, veterinarians, and meat industry workers due to contact with infected reproductive tissues, unpasteurized milk, or animal fluids. The infection in humans manifests as chills, fever, weakness, fatigue, and other flu-like symptoms, and it is also known as undulant fever due to its intermittent nature. Brucellosis is caused by the bacterium Brucella, which can affect a wide variety of animals including cattle, pigs, sheep, goats, horses, and dogs. Brucella organisms can be present in birthing tissues or fluids (aborted fetuses, fetal fluids, placentas, and vaginal discharges), and also in milk, urine, blood, and semen. Transmission among cattle is through ingestion of birthing fluids and milk and in utero. The most common clinical sign in cattle is late-term abortion, but many infected cattle do not show any clinical signs. Most infections in humans are associated with drinking or eating unpasteurized milk products. Handling infected aborted fetuses or after birth is another common means of human infection, as the organism can enter through cuts in the skin and the mucous membranes of the eye and mouth. Common symptoms in humans are undulating fever, weakness, headache, joint pain, and night sweats. Human brucellosis is prevented by not drinking unpasteurized dairy products and wearing gloves when handling reproductive tissues. Hands should be washed after touching or handling animals.
Campylobacteriosis
Campylobacter is a major cause of gastroenteritis globally, often found in poultry and other farm animals. The bacterium is present in the intestines of animals, often without causing disease, though it can lead to abortions in sheep. Humans are typically infected through the consumption of contaminated or undercooked meat, particularly poultry, or unpasteurized milk. Symptoms of Campylobacter infection include diarrhea, abdominal pain, fever, nausea, and vomiting. In rare cases, it can lead to complications such as Guillain-Barre syndrome.
Cryptosporidiosis
Cryptosporidiosis is a parasitic infection caused by Cryptosporidium, most commonly observed in calves less than one month old. The parasite is shed in the feces of infected animals, contaminating food or water. Humans contract the infection through the consumption of contaminated water or food, or through direct contact with infected animals. Symptoms include diarrhea, abdominal pain, vomiting, and fever, with severe cases more likely in young children, pregnant women, and immunocompromised individuals. Preventative measures focus on hygiene and disinfection.
Listeriosis
Listeriosis, caused by Listeria monocytogenes, is associated with the consumption of contaminated food, particularly soft cheeses and processed meats. The bacterium can grow at low temperatures, and infections are often linked to refrigerated products. Clinical symptoms include fever, headache, nausea, and, in severe cases, sepsis, meningitis, and miscarriages. Listeria can also contaminate dairy products and vegetables, with outbreaks frequently linked to raw or unpasteurized foods.
Leptospirosis
Leptospirosis is a bacterial disease caused by Leptospira interrogans, which affects a wide range of animals and is spread through their urine. Infected cattle and rodents can shed the bacteria without showing symptoms. Humans acquire the disease through contact with contaminated water or soil, leading to mild flu-like symptoms or, in severe cases, liver and kidney failure. Prevention includes controlling rodents and avoiding stagnant water.
Q Fever
Q fever, caused by Coxiella burnetii, can lead to abortions in cattle, sheep, and goats. Humans typically acquire Q fever through contact with reproductive fluids or milk from infected animals. Symptoms in humans range from fever and night sweats to severe pneumonia and hepatitis. Preventative measures include handling abortion cases carefully and avoiding unpasteurized dairy products.
Toxoplasmosis
Toxoplasma gondii is a widespread protozoan parasite infecting both animals and humans. Transmission to humans occurs through contact with cat feces or consumption of undercooked meat containing the parasite’s tissue cysts. Toxoplasmosis can cause serious complications, including encephalitis and abortion, especially in pregnant women. Preventative measures include proper handling of cat litter and cooking meat thoroughly.
References:
Bidaisee, S. and Macpherson, C.N.L. (2014). Zoonoses and One Health: A Review of the Literature. Journal of Parasitology Research, 1: 1-8.
Okeleji, L.O., Ajayi, L.O., Odeyemi, A.N., Amos, V., Akanbi, B.G., Onaolapo, M.C., et al., (2024). Bacterial Zoonotic Diseases and Male Reproduction. Zoonotic Diseases, 4: 97-113.
Rahman, M.T, Sobur, M.A., Islam, M.S., Ievy, S., Hossain, M.J., El Zowalaty, M.E, et al., (2020). Diseases: Etiology, Impact, and Control. Microorganisms. 8(9):1405.
United Nations Environment Programme and International Livestock Research Institute (2020). Preventing the next pandemic: Zoonotic diseases and how to break the chain of transmission. Nairobi, Kenya: UNEP.
Woolhouse, M.E, Gowtage-Sequeria, S. (2005). Host range and emerging and reemerging pathogens. Emergency Infectious Diseases, 11(12):1842-1847.